To estimate the cost of building a website or an app, use our app cost calculator tool.
Despite the rapid digitization of healthcare, one critical challenge remains unresolved: patient data is still profoundly fragmented.
Medical records are scattered across electronic health systems, lab databases, imaging archives, and even personal wearables. They are rarely connected in a way that gives providers a complete picture.
This fragmentation isn't just inconvenient. It creates blind spots that can delay diagnoses, increase costs, and put patient outcomes at risk.
For healthcare organizations striving to improve diagnostic accuracy and streamline workflows, this is a major barrier.
Artificial Intelligence (AI) is emerging as a powerful solution.
It transforms disconnected datasets into unified, actionable insights that support more accurate, timely, and personalized care.
In this article, we’ll explore the real cost of fragmented healthcare data and how AI is reshaping diagnostics for a more connected, patient-centered future.
What is Fragmented Healthcare Data?
Fragmented data in healthcare refers to the systemic separation of patient information across institutions, departments, and technologies that rarely speak the same language.
Even within a single health system, data may be housed in incompatible formats—structured in one department, unstructured in another, or locked behind vendor-specific barriers.
This lack of fluidity creates invisible walls around patient records. It forces providers to make decisions with only partial histories and limits the potential for AI-driven insights that rely on comprehensive datasets.
Much of the fragmentation stems from a broader issue: the healthcare ecosystem is built on a patchwork of IT systems, each developed in isolation.
With no universal data standards, organizations adopt platforms based on short-term operational needs, not long-term interoperability.
The result is a deeply siloed infrastructure, where data portability remains the exception, not the norm.
How Fragmented Healthcare Data Impacts Diagnosis?
Diagnosing a condition isn’t just about checking one symptom or test result.
It’s about seeing the whole picture: how a patient’s health has changed over time, how treatments have worked (or haven’t), and where subtle patterns might reveal bigger concerns.
But doctors are left filling in the gaps when that information is spread across disconnected systems.
Let’s take a closer look at the areas where fragmented data most directly affects diagnosis.
1. Chronic Disease Management
A patient with diabetes visiting multiple clinics may have inconsistent records of blood sugar levels, lab tests, and prescribed medications at different health facilities. This will cause their physicians to either duplicate tests or miss critical trends.
2. Emergency Situations
In emergency care, such as a heart attack, if the care team does not have access to a patient’s history of cardiac issues or allergies to medication, it can result in suboptimal or harmful treatment decisions.
3. Cancer Diagnosis and Treatment
As highlighted by a 2024 study in BMC Health Services Research (Source), a lack of shared records across oncology specialists and primary care providers can delay diagnosis or lead to inappropriate treatment strategies.
Limitations of Traditional Diagnostic Tools
Traditional diagnostic tools, although innovative at the time of their creation, fall short of addressing fragmented data because:
1. They don’t integrate information across platforms
Most traditional tools operate independently and are unable to combine data from multiple platforms, systems, or healthcare providers effectively.
2. They can’t interpret incomplete data
Diagnostic algorithms may misinterpret isolated data points without access to integrated patient histories, leading to inaccuracies.
3. They don’t support real-time decision-making
The manual processes of traditional tools slow down data collection and analysis, making it challenging to provide timely insights for critical diagnoses.
Diagnostic Challenges Caused by Fragmented Data
Now that we’ve seen where fragmented data has the most impact, let’s look at the specific diagnostic challenges it creates.

1. Increased Hospitalization
One of the most noticeable effects of fragmented healthcare data is a rise in hospital visits, especially for patients with multiple chronic conditions.
When your doctors cannot access your complete medical history, they may miss early warning signs or make less informed decisions.
A 2018 Commonwealth Fund study (Source) found that Medicare patients with 3 to 4 chronic illnesses and fragmented care were 14% more likely to visit the emergency room and 6% more likely to be hospitalized.
Even with just one condition, you face a 14% higher risk of hospital admission compared to patients receiving more coordinated care.
2. Redundant Testing and Increased Costs
When providers don’t have access to previous test results, they’re often forced to repeat diagnostics—just to be safe. This is especially common with imaging scans, lab panels, and blood work.
Redundant testing doesn't just drive up costs. It also strains lab capacity, increases patient burden, and delays time to treatment while clinicians wait for results that already exist elsewhere.
According to a study published in JAMA Internal Medicine, as much as 20% of laboratory tests may be unnecessary, often due to information gaps or lack of system integration.
Preventing this kind of waste requires more than electronic records. It demands seamless data sharing and intelligent systems that surface relevant patient history at the point of care.
3. Delayed Diagnoses
Every moment counts when dealing with a chronic or progressive condition. Delays in diagnosis can give the illness time to worsen, making treatment less effective.
Imagine getting a scan for a suspicious growth, only to learn your specialist can’t access the images because of incompatible systems.
That lost time could mean a missed opportunity for early, life-saving care.
When your medical data isn’t easily accessible, doctors spend valuable time tracking it down instead of treating you.
4. Inconsistent Healthcare Plans
If you’re managing a chronic condition like diabetes or rheumatoid arthritis, you likely see several specialists, each focused on a different part of your health.
But when these providers don’t share a unified view of your medical history, their care plans can overlap, conflict, or even work against each other.
Treatment decisions may clash without coordination, leading to confusion or even unintended harm.
Key AI Strategies for Addressing Fragmented Healthcare Data
AI integrates disparate data sources, making them interoperable, actionable, and insightful.
Through its cutting-edge tools like machine learning (ML), natural language processing (NLP), and deep learning, AI automates data extraction, analysis, and integration across siloed systems, addressing messy data fragmentation with precision.
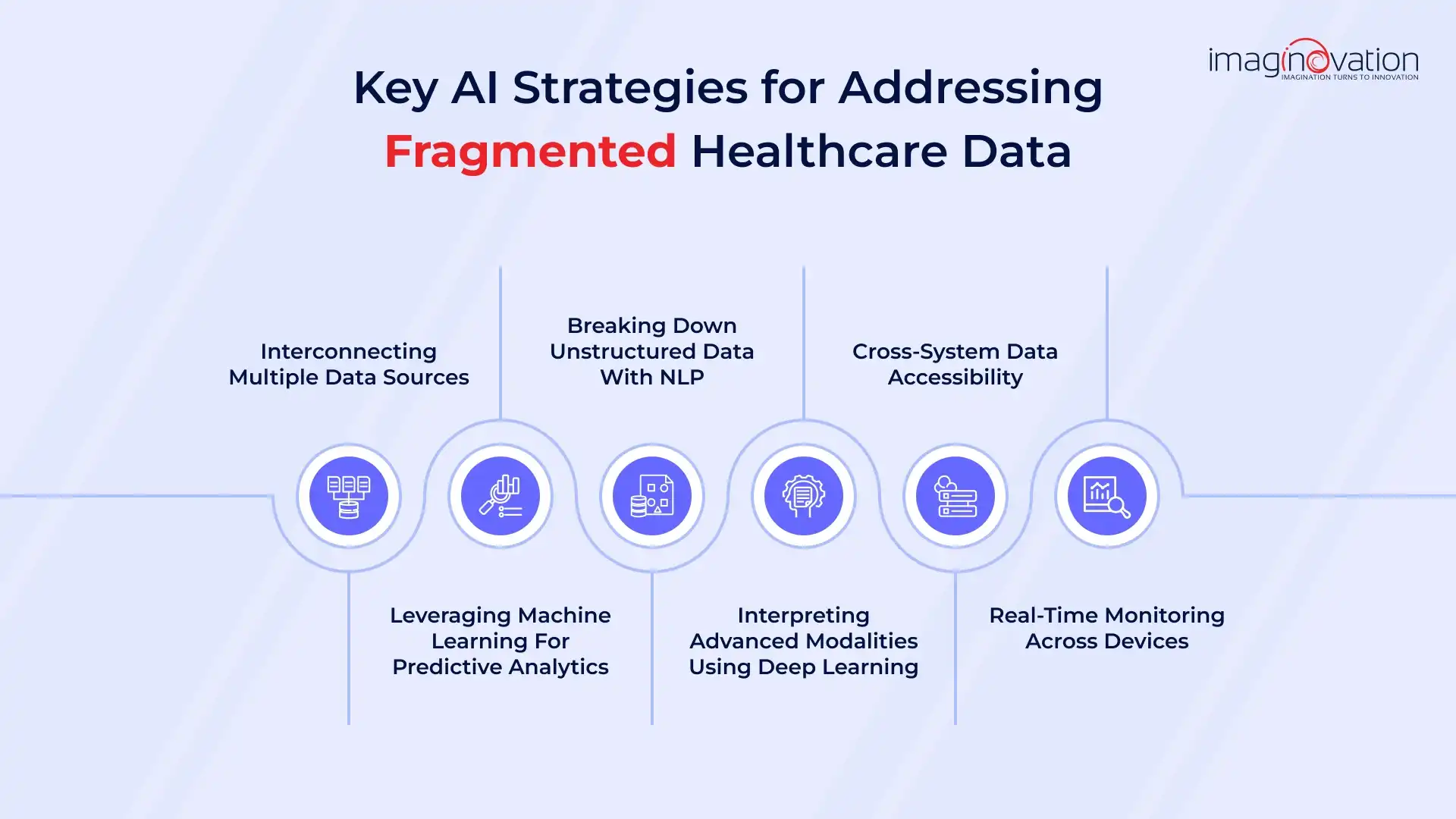
1. Interconnecting multiple data sources
AI helps you connect the dots across disconnected systems. It pulls data from labs, imaging, pharmacies, and even wearable devices and combines it into one clear, unified patient record.
Take IBM Watson Health, for example. It brings together information from multiple EHRs into a single, easy-to-use dashboard, giving you a complete 360° view of your patient’s health.
2. Leveraging Machine Learning for predictive analytics
Machine learning (ML) identifies patterns and correlations in fragmented datasets. For example, ML algorithms analyze data across patient populations to predict risks like hospital readmissions or complications, enabling proactive intervention.
As per Statista, 72% of healthcare leaders worldwide acknowledged the positive influence of predictive analytics on patient health outcomes.
3. Breaking down unstructured data with NLP
Natural language processing (NLP) transforms unstructured data in the form of physician notes, discharge summaries, insurance claims, and other scanned documents into structured formats.
For instance, Google Health's AI uses NLP to extract meaningful insights from physician notes, making diagnoses and treatment plans accessible on a larger scale.
4. Interpreting advanced modalities using Deep Learning
Deep learning processes complex data types, such as medical imaging and genomics, integrating them with other records for comprehensive diagnostics.
AI platforms like Aidoc analyze CT scans alongside patient histories, creating insights that reduce diagnostic fragmentation and improve accuracy.
5. Cross-system data accessibility
AI integrates data from legacy systems and third-party software, enabling healthcare organizations to overcome interoperability issues.
For example, FHIR (Fast Healthcare Interoperability Resources) standards, supplemented by AI tools, allow different systems to exchange patient data seamlessly, reducing bottlenecks in care coordination.
6. Real-time monitoring across devices
Wearables, IoT devices, and continuous monitoring systems generate massive amounts of raw data. AI aggregates this data and links it with clinical records for real-time analysis.
For example, Apple’s HealthKit integrates wearable data with EHR platforms, providing uninterrupted insights into patient health.
Operational Benefits of AI Integration for Improved Diagnosis
Integrating AI into diagnostic processes yields measurable outcomes and strategic advantages that healthcare organizations can leverage for improved patient care and operational efficiency.
Key benefits include:

1. Enhanced Diagnostic Accuracy
AI medical diagnosis helps you find issues early and accurately. It spots patterns in scans and records that doctors might miss, reducing errors and improving patient outcomes.
2. Improved Speed and Proactive Disease Detection
AI tools help you detect diseases faster by analyzing data in real-time. This means your doctor can act quickly, start treatment sooner, and stop the disease from getting worse.
3. Increased Efficiency and Productivity
AI takes care of repetitive tasks and gathers data automatically. This gives you more time to focus on patient care. It also helps your team work faster and more efficiently. You can make clearer, more consistent decisions with all patient data in one place.
4. Significant Cost Savings
AI helps you avoid diagnostic errors and unnecessary tests. This cuts down on wasted time and resources. Faster, more accurate diagnoses mean shorter hospital stays and fewer readmissions. That leads to steady savings for your organization.
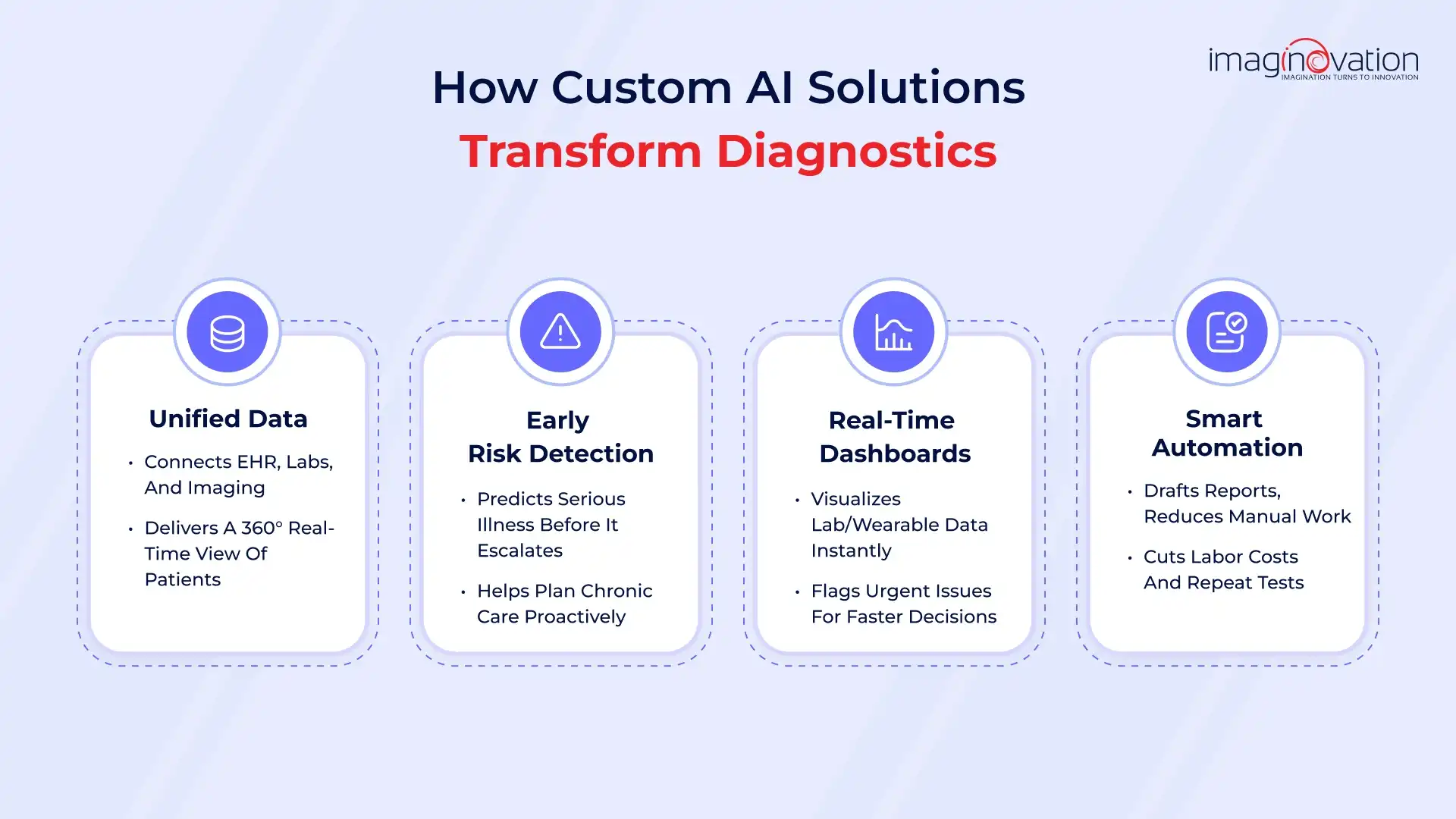
Opportunities for Healthcare Organizations Using Custom AI Solutions
Many healthcare organizations turn to custom-built AI solutions because of the benefits they offer. Here are a few ways you can use AI technology in the health sector.
1. Enhanced accuracy in diagnostics.
Healthcare often runs in silos. That means your patient data can be scattered across systems—EHRs, labs, imaging, and more. You don’t always have the full picture when you need it.
AI can fix that. By building an AI-powered platform, you can combine data from all these sources into one place. This gives you a real-time, complete view of each patient.
What do you gain?
Better diagnostic accuracy: When all the data is in one place, you're less likely to miss something important. That means fewer misdiagnoses and faster, more confident decisions.
Smooth coordination: AI ensures seamless communication between departments. Everyone from radiologists to primary care providers sees the same up-to-date information.
Cleaner records: A Master Patient Index (MPI) powered by AI removes duplicates and matches records accurately. You get reliable, consistent data every time.
2. Improved speed and effectiveness in disease detection.
AI helps you find high-risk patients faster. It looks at both past and real-time data to predict if someone might get seriously sick. You can catch diseases before they become urgent problems.
What do you gain?
- Early warning signs so you can act fast.
- Less strain on emergency care.
- Better planning and support for chronic illnesses.
3. Increased efficiency and productivity.
AI dashboards help you see key patient data fast. They collect and process real-time info from wearables and lab tests, then show it in clear, easy-to-read visuals. You get instant insights without digging through files and spotting urgent issues.
What do you gain?
- Faster decisions with real-time updates.
- Better teamwork using shared, visual insights.
4. Significant cost savings.
AI can pull insights from raw data like lab reports or imaging results. It also automates routine tasks like report writing and record-keeping.
For example, your radiology team scans and interprets medical images using AI. It creates first-draft reports instantly so radiologists can review them faster and move on to the next case.
What do you gain?
- Fewer manual errors and faster test results.
- More time to focus on your patients, not paperwork.
- Lower labor costs and fewer repeat tests.
Overcoming Implementation Challenges with Custom Solutions
As you consider upgrading to AI-powered diagnostics, take note of the list of challenges you may face:
1. Data Quality and Availability Concerns
AI tools require clean, high-quality, and consistent data. However, healthcare data is often siloed, incomplete, inaccurate, and missing key details, leading to unreliable AI models. To ensure effective AI solutions, ensure your data is complete, standardized, and reliable.
2. Integration with Legacy Systems
Hospitals often rely on a mix of outdated and modern software, which can make integrating AI into these systems challenging. To maximize the value of AI, you need strong APIs and standards like FHIR to ensure smooth integration, especially with EHRs and imaging systems.
3. Privacy and Security Risks
Handling sensitive patient data makes your systems prime targets for cyberattacks. A breach can result in identity theft, fraud, and harm to patient care. AI needs access to large volumes of data, raising security risks if data protections on your AI solution aren’t robust enough.
4. Regulatory and Ethical Compliance
AI in healthcare must comply with regulations like FDA approvals for diagnostic tools and HIPAA laws for patient privacy. Addressing ethical concerns such as bias, transparency, and accountability is also crucial. Stay up to date with evolving regulations to maintain compliance.
5. High Development Costs and ROI Concerns
Custom AI solutions are expensive to develop and require skilled experts and significant resources. Without a clear ROI strategy, it can be challenging to justify these costs, making stakeholders hesitant to commit to long-term adoption.
At Imaginovation, we know that successful AI medical diagnosis isn't just about advanced algorithms — it’s about building trust, ensuring precision, and making tools easy for your teams to use.
That’s why we design AI solutions around your clinicians, not the other way around.
Our human-centered design approach ensures that adoption feels natural. From the start, we focus on regulatory-first engineering — compliance with HIPAA, FDA, and global data standards to protect patient data and minimize legal risk.
Our smart, modular architecture lets you scale your customized AI systems as your needs grow, without reworking your entire tech stack.
Best of all, we ensure AI isn't just added to your system; it’s seamlessly woven into it.
Conclusion
Driven by the power of AI technology, healthcare is on the brink of a major transformation.
AI-powered solutions are improving clinical decisions, streamlining administrative tasks, and accelerating research. They also help you deliver more personalized care.
To unlock real value, you need to address implementation challenges and follow proven best practices. AI helps you save time, reduce errors, and spark innovation.
This isn’t just about upgrading your tools—it’s about building a smarter, more responsive, and patient-centered future.
Ready to lead the way?
Get in touch with us at Imaginovation and explore how we can help you use AI to reshape your healthcare operations.