To estimate the cost of building a website or an app, use our app cost calculator tool.
Isn’t it exciting when your healthcare software is finally in development, and you’re counting down to the big launch?
But then you keep hearing, “We just need two more weeks to finish it.” And the worst part is that they’ve been saying that for six months.
If that sounds familiar, we hear you. A huge number of healthcare software projects fall apart simply because the wrong vendor was at the wheel. In fact, studies show that up to 70% of healthcare technology projects fail due to cost overruns, poor usability, or low adoption.
We’ve been called in countless times to rescue applications that veered completely off track. Failed EHR integrations, clunky patient portals, systems no one can actually use, we've fixed them all.
But we're not here for a vendor-blaming rant.
In this blog, we’re going to break down how to fix healthcare software that was derailed by a previous vendor and how you can relaunch it successfully.
Let’s get started.
How Bad Vendors Kill Healthcare Software Projects
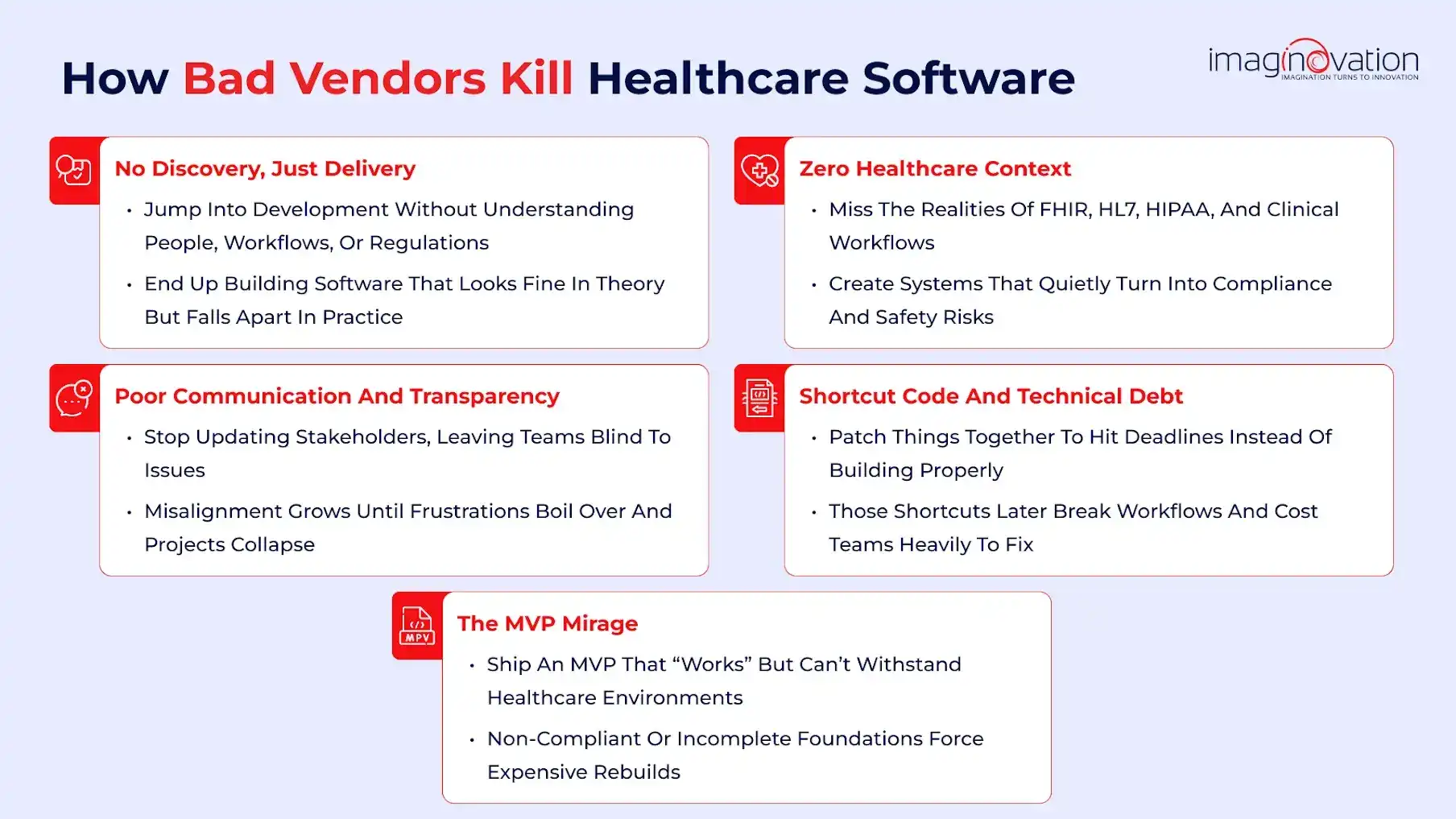
Healthcare software projects must be developed with precision and care.
Organizations need to take a strategic lens to diagnose the root causes of failure, helping them better understand their vendors and make more intelligent choices.
Here’s a glimpse into the chaos many healthcare teams face.
1. No Discovery, Just Delivery
Many vendors get straight into development without investing enough time in discovery.
They skip critical steps, such as stakeholder interviews and workflow and regulatory scoping. The result, as expected, is software that looks good on paper but collapses in practice.
Real Example:
Girard Medical Center in Kansas wanted to implement an EHR system and signed a $2.9 million contract with Cerner, one of the top EHR vendors.
The vendor never fully understood the hospital’s size or workflows, and the system never went live.
The hospital had been waiting for over a year and a half, lost over $1 million, and missed federal incentives.
According to Girard's filing, they admitted that the hospital had provided notice to Cerner on several occasions and that it was not fulfilling its promises. This is a classic case of skipping discovery and building blind. (Source)
2. Zero Healthcare Context
Healthcare isn’t like fintech or retail. It has its own ecosystem of standards, such as FHIR, HL7, and HIPAA, that govern how data flows and privacy is protected.
Vendors without this context create ticking compliance time bombs.
In this context, Pete Peranzo, Co-founder of Imaginovation, shares, "The biggest hurdle that companies face with these healthcare-type applications is compliance. There's just so much compliance that it slows everything down."
Real Example:
The U.S. Department of Veterans Affairs and Oracle Cerner EHR rollout exposed this gap dramatically.
The system routed more than 11,000 patient orders to an “unknown queue,” resulting in delays in care and documented patient harm.
The flaw was called an apparent failure and attributed to a lack of domain understanding and testing rigor.
Source: DOTMed Report
3. Poor Communication and Transparency
What happens when communication breaks down?
Trust erodes, and quite often, by the time clients realize something is wrong, it’s usually too late.
Real Example:
A hospital in a published ResearchGate case study returned to paper workflows after its EHR rollout failed. The cause wasn’t just bad code; it was poor communication.
When developers stopped updating stakeholders, leadership had no visibility, and users’ frustrations went unheard until the entire project collapsed.
Source: ResearchGate Study
4. Shortcut Code and Technical Debt
Rushing to meet unrealistic deadlines, vendors often “make it work” with quick fixes.
But in healthcare, those shortcuts don’t just break software, but also risk patient safety.
Real Example:
During the VA’s Oracle Cerner deployment, internal investigations revealed technical patches and untested modules that triggered major workflow failures.
Orders went missing, alerts failed, and clinicians lost faith in the system. The resulting technical debt cost millions to unwind.
Source: NextGov Report
5. The MVP Mirage
The “fast MVP” promise can be deceptive. Vendors deliver something that looks usable, but lacks the robustness for real-world healthcare environments.
Real Example:
A wellness startup building a remote patient monitoring platform rushed to launch an MVP . The vendor used non-compliant APIs, ignoring FHIR standards. When hospitals finally got ready to pilot the system, it failed interoperability testing.
The entire product had to be rebuilt from scratch, and it turned out to be a costly lesson.
👉 Bottom line
Most failed healthcare software projects don’t just fail overnight; they collapse quietly under poor processes.
Other factors, such as poor communication and misplaced priorities, also contribute to the failure. Each delay, shortcut, and misstep compounds until the system, and the trust collapses.
💡 Imaginovation Insight
When it comes to the most common mistakes healthcare leaders make when choosing a software development vendor, Pete underscores, "Procurement missteps, rushing RFPs, prioritizing cost over capability, and ignoring compliance expertise are common pitfalls that can severely impact healthcare software projects."
Pete adds, "The biggest one that we've \[Imaginovation] experienced is that the difference between us and other companies is that a lot of these companies, especially in this space, they'll build you a system and then they lease it out to you. So you technically don't own the full product."
He sums up, "You need a vendor that has niche experience working in the healthcare space, dealing with FDA approvals and HIPAA compliance, but also one that doesn't sacrifice user experience and speed."
What Great Healthcare Software Developers Do Differently?
For healthcare leaders ready to seize the moment, developing future-proof healthcare software is essential. Finding a reliable and expert partner can make all the difference.
Here’s a glimpse of the opportunities you can unlock with the right partner guiding your healthcare software project.
1. Discovery-First, Always
Top partners have a systematic process for asking the tough questions. The discovery process is detailed, helping to understand the project thoroughly before writing a single line of code.
They invest time in understanding workflows, user needs, and regulatory constraints. This background work helps to ensure that development starts on solid ground.
2. Compliance-Led Thinking
They design with HIPAA, PHI, and clinical validation built in from the beginning, not added as an afterthought.
3. Clear Documentation and Ownership
All stakeholders have visibility, which is ensured through transparent code repositories.
Moreover, the partners work on structured handoffs and open collaboration. These steps are taken to ensure accountability throughout the project lifecycle.
4. Empathy for the End User
Every feature is tied to clinical or patient workflows, not just developer convenience, making the software truly usable in real-world settings.
5. Long-Term Thinking
Architecture is designed with the heart to ensure scalability and maintainability. The development team will never build healthcare software projects for short-term sprints or quick fixes.
When rebuilding a failed healthcare software project, Pete shares what the Imaginovation team does differently. Pete reiterates, “The Imaginovation team differentiates itself from other companies primarily through ownership and control of the software they develop. Unlike many vendors who build systems and lease them out, Imaginovation ensures that its clients own the whole intellectual property (IP) of the product. This approach provides clients with full ownership rights, enabling better flexibility and control over the software, especially if they need to transition away from a previous vendor.”
He underscores his point through the case study of Everflex, a successful custom healthcare software system rebuilt by the Imaginovation team. The case involved partnering with Movement for Life, a unique private practice physical therapy company, to effectively reconstruct their software— demonstrating Imaginovation’s expertise in delivering thorough, high-quality solutions.
Everflex exemplified Imaginovation’s ability to revitalize and enhance healthcare software systems, showcasing the team’s proficiency in managing complex projects and turning around legacy or problematic software solutions for healthcare clients.
How to Fix Broken Healthcare Projects for Good

Here's a surefire way to rescue and future-proof a failing healthcare software project.
Step 1: Audit Existing Project
You cannot fix without knowing what needs fixing.
Therefore, it is a great idea to do a full-fledged audit on both technical and compliance aspects.
Among the factors that need audit are code quality, infrastructure, and data governance. You can give a thought to identify what’s salvageable and what constitutes technical debt.
Remember to check review contracts, documentation, and access controls.
👉 Key takeaway: It will help to get a clear picture of the extent of the rescue, so that you can work around it.
Step 2: Reconsider Your Development Partners
When selecting the right delivery partner, one must remember that it is a strategic decision. It is best not to consider it as a procurement exercise.
Ask the questions that reveal real capability:
- How is healthcare compliance embedded in your architecture?
- Who owns the code and IP?
- What’s your discovery and handoff process?
👉 Watch for red flags:
There are clear red flags to watch out for, such as unclear accountability or weak processes. Yet another red flag is evasive communication.
👉 Mindset:
When choosing partners, remember the focus should be on working towards long-term transformation partners.
Step 3: Redefine Discovery
In this stage, you must take in stride the broken projects that are most often based on poor discovery and work to redo them. It is also great to reconfirm business goals, workflows, and clinical outcomes.
All leaders, from clinical to operational to IT, must be in alignment. Further, the focus can be on defining compliance checkpoints and critical paths before design begins.
👉 Insight: It is worth noting that robust discovery prevents 80% of rebuild costs later.
Step 4: Plan, Don’t Patch
In the next stage, it will help to adopt a structured recovery roadmap that focuses on stabilizing the software project. The development team can then work together to redesign the project.
As the stage shapes up, one needs to work on redeployment. During this stage, it is vital to prioritize high-risk areas, including data integrity and user experience.
Yet another facet to work on is allocating the budget for validation and testing, in addition to coding.
👉 Imaginovation Insight:
Imaginovation’s experience has been that teams often spend less time rebuilding correctly than endlessly patching flawed systems.
Step 5: Redesign and Develop the Right Way
When redesigning, remember to modernize the software project, keep scalability in mind. It is vital to have a tight check on building security features and to keep sustainability in mind.
A great way will be to use agile sprints with transparent milestones. The development team can embed compliance monitoring from day one.
At every stage, document all technical and design decisions.
👉 Imaginovation edge:
At Imaginovation, we enforce developer accountability, ensure transparency of ownership, and maintain governance throughout the build.
Step 6: Validate, Test, and Govern
The QA and Testing phase is crucial, and the software project must go through rigorous validation with long-term oversight.
The vendor must ensure the project goes through continuous QA and HIPAA/FDA compliance checks. It will be great to have independent audits before production.
When it comes to ongoing governance, make sure to include:
- Regular compliance audits
- Change-management protocols
- Vendor performance tracking
Final Takeaway:
Broken healthcare projects can be revived, but only with disciplined auditing, transparent partnerships, and governance built in from the start.
Imaginovation’s proven recovery framework ensures that your next deployment is secure, scalable, and built to last.
Wrapping Up: Your Vendor Failed, Not Your Vision
When a project fails, you can either mull over your strategy going wrong or reconsider whether you’ve looped in the wrong vendor.
The good news: many healthcare organizations have rebuilt stronger systems after setbacks by taking things in stride, reassessing what went wrong, and aligning business goals with technology delivery.
If you, too, are dealing with a failed or stalled healthcare software project, you may start with a quick audit. Our team at Imaginovation can help you uncover what’s fixable and reignite the vision you started with.
We have extensive experience in building, integrating, and scaling the right solutions with confidence.