To estimate the cost of building a website or an app, use our app cost calculator tool.
Data is the foundation of modern healthcare. It drives critical decisions about treatment plans, patient care, and resource management.
However, poor data quality in healthcare remains a major challenge. Simple typos, duplicate records, or missing information often result in medical errors, delays in care, and even life-threatening situations.
Yet, fixing these issues manually is a time-consuming and never-ending task. Analysts spend up to 80% of their time cleaning data instead of analyzing it.
Modern technology has transformed healthcare, enabling better treatments and collaboration.
But without high-quality data, even the best technology falls short. A single misplaced decimal, missing digit or inconsistent terminology can corrupt entire datasets, leading to costly mistakes.
This is where AI and automation come in.
By detecting, correcting, and preventing data errors at scale, these technologies can transform unreliable data into a valuable asset—improving accuracy, efficiency, and, ultimately, patient outcomes.
Let's explore how AI and automation can fix healthcare data quality.
Importance of Data Quality in Healthcare
Reliable and accurate data is important in healthcare to ensure proper diagnosis, treatment, and patient safety.
Here are key areas where data issues create risks:
1. Duplicate Patient Records
Duplicate records occur when a single patient is represented multiple times in a database. This issue typically arises from inconsistent data collection methods or suboptimal matching algorithms that fail to accurately link records.
When patient information is split across multiple profiles, it fragments the complete medical history, making it harder for healthcare providers to access comprehensive data. This can lead to delayed diagnoses, fragmented care, and increased risk of medical errors.
2. Inaccurate/Incomplete Data
Inaccurate or incomplete data occurs when errors in data entry lead to incorrect or missing patient details and medical histories.
Such errors compromise data integrity and can expose healthcare organizations to legal risks, financial losses, and malpractice liabilities.
Moreover, these issues disrupt clinical workflows by necessitating additional verification and corrections, ultimately delaying patient care.
3. Inconsistent Terminologies
Healthcare providers often use varied terminologies and coding standards, leading to data mismatches and miscommunication that can compromise patient outcomes.
For example, when integrating data across multiple departments, one system might utilize ICD-10 codes while another uses SNOMED CT. These differing standards can create discrepancies in how conditions are recorded, such as using slightly different terms or codes for the same diagnosis.
4. Outdated Information
Patient records that are not regularly updated can contain outdated information, which poses serious risks to patient care. Over time, treatment plans, medications, and health conditions evolve.
When healthcare providers rely on obsolete data, it can lead to inappropriate or ineffective treatment strategies—particularly in chronic disease management, where up-to-date information is critical.
Outdated information can also hinder timely interventions, impacting patient safety and overall care quality.
5. Data Integration Challenges
Healthcare organizations gather data from diverse sources, such as Electronic Health Records (EHRs), medical devices, and laboratory systems. Integrating this data can be challenging when it is stored in various formats and structures.
These discrepancies often lead to inconsistencies, duplication, or missing data, undermining the overall dataset's reliability. Such challenges hinder seamless data exchange and can complicate clinical decision-making.
Also Read: Healthcare Software Development: A Complete Guide
Why Do Traditional Data Management Strategies Fail?
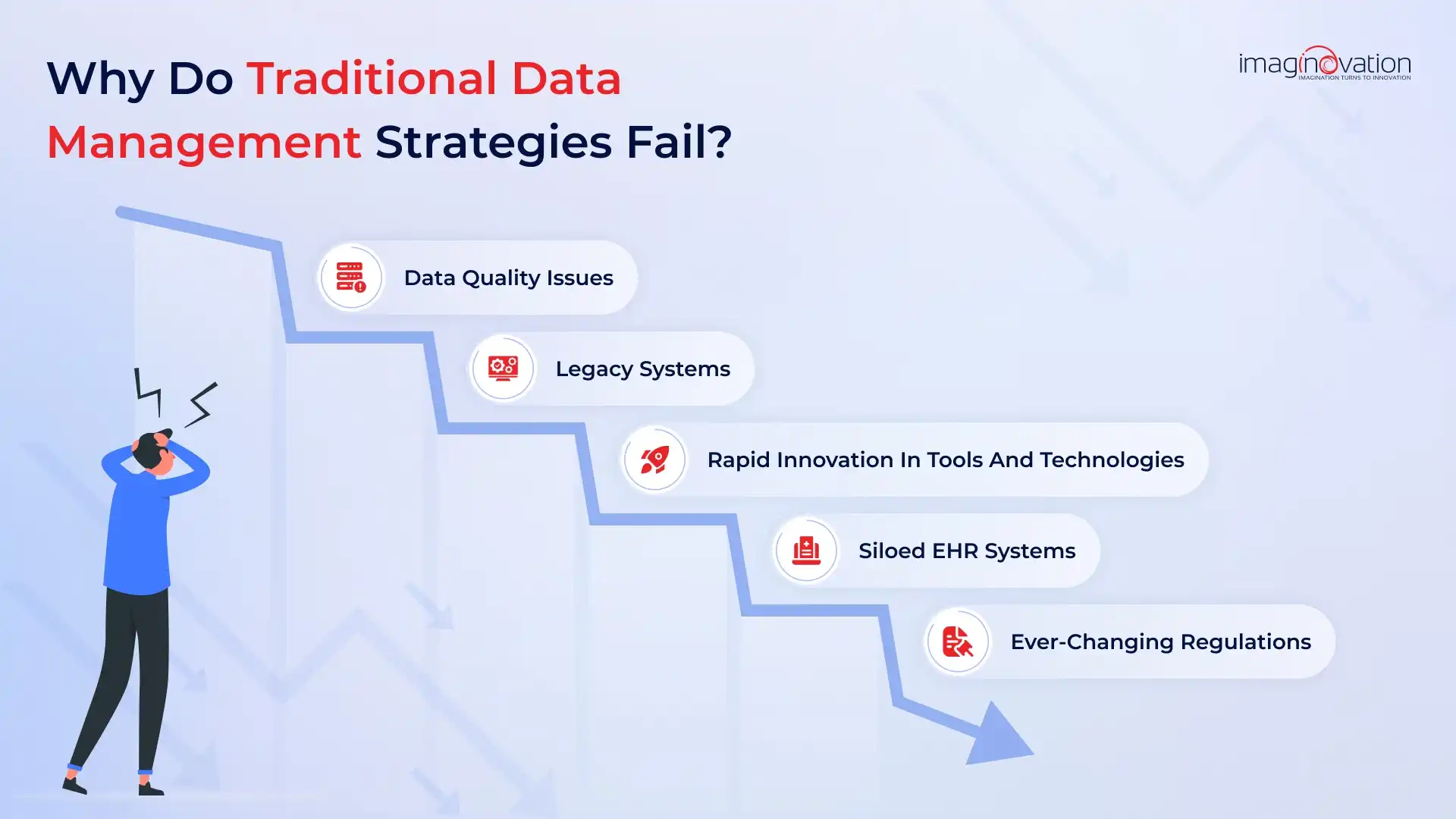
Traditional data management in healthcare often relies on manual processes and legacy systems that are ill-equipped to handle today’s vast and evolving data demands.
These outdated approaches hinder accurate data capture, analysis, and seamless integration, ultimately affecting patient care and operational efficiency.
Let's take a look at the key challenges:
1. Data Quality Issues
Manual data entry and processing frequently lead to inconsistencies, duplications, and incomplete records.
Studies have indicated error rates can be as high as 27% in some healthcare settings, according to a study by the Journal of the American Medical Informatics Association. The 1-10-100 Quality Principle further illustrates that addressing issues at data entry is far more cost-effective than dealing with them later.
Moreover, repetitive manual tasks can burden a significant portion of the workforce, diverting time from critical patient care.
2. Legacy Systems
Decades-old legacy systems often harbor unstructured and uncleaned data. These rigid architectures are not designed for real-time validation or seamless integration with modern technologies.
Their inability to support large-scale applications and integrate with open-source solutions further impedes effective data-driven decision-making.
3. Rapidly Evolving Tools and Technologies
As the healthcare technology landscape evolves, traditional systems struggle to keep pace. Budget constraints and compatibility issues between legacy systems and modern tools limit comprehensive data analysis.
Continuous investment in training and modern data solutions is essential to leverage new technologies and enhance overall insights and patient outcomes.
3. Siloed EHR Systems
Many healthcare organizations operate with siloed Electronic Health Record (EHR) systems that store patient data separately. This fragmentation can result in incomplete records, redundant tests, and delayed diagnoses, as specialists may not have access to a complete patient history.
Adopting interoperability standards and cloud-based integration tools can break down these silos and foster more collaborative care.
4. Ever-Changing Regulations
Healthcare data management must comply with strict and frequently evolving regulatory requirements. Traditional systems, with their manual update processes and inflexible structures, often fail to adapt to these changes.
This lag not only increases the risk of non-compliance and potential penalties but also undermines patient trust.
Modern data platforms, with built-in automation and flexible controls, are better suited to meet these dynamic regulatory demands.
How AI & Automation Can Fix Poor Data Quality Issues
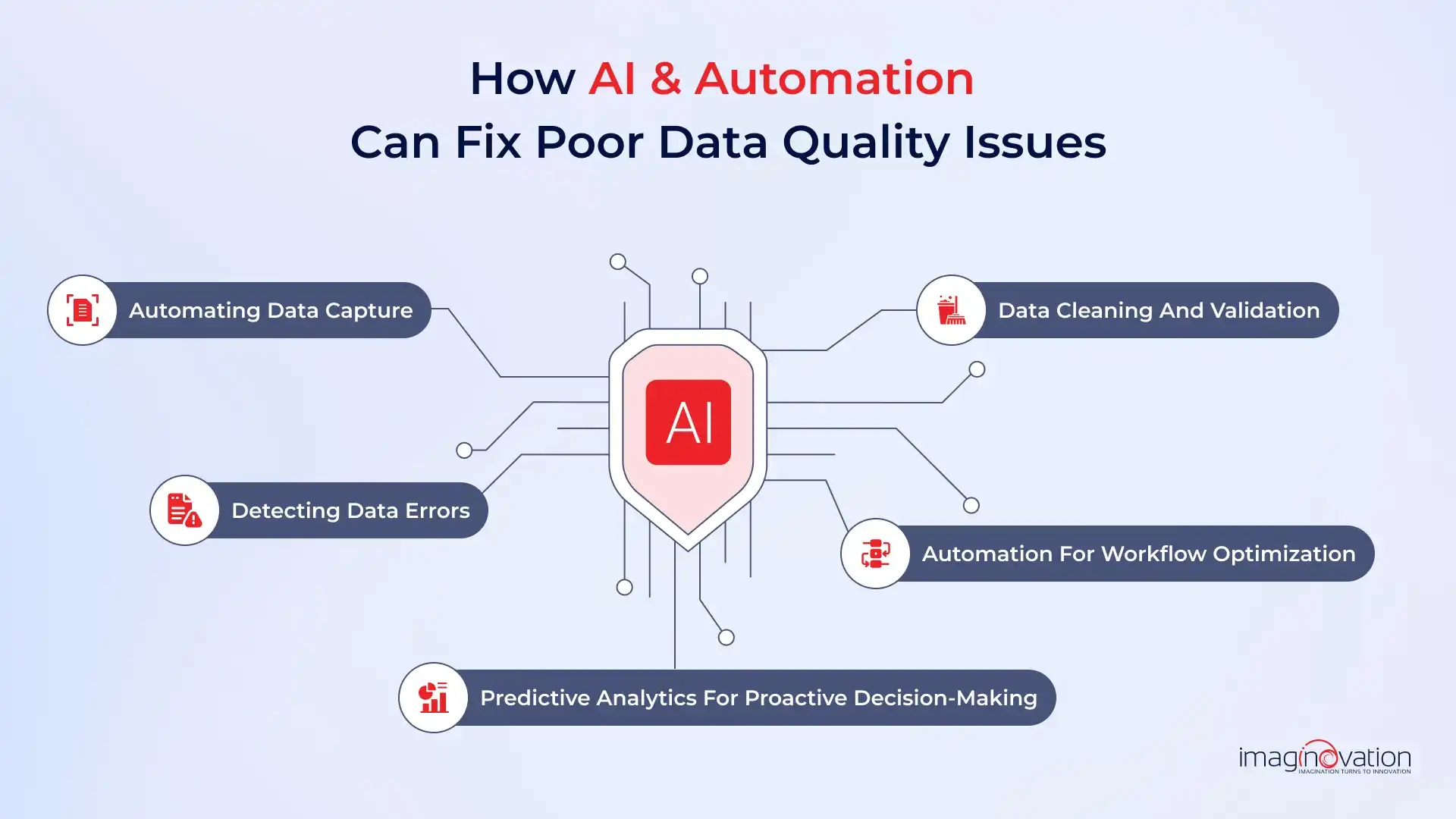
In busy healthcare settings, data accumulates rapidly, often resulting in “data waste” from errors, duplicates, and inconsistencies. Poor data quality leads to lost opportunities, flawed insights, and wasted resources.
Fortunately, Artificial Intelligence (AI) and Machine Learning (ML) can help by automating data cleaning, monitoring, and optimization. These technologies enhance accuracy, consistency, and efficiency.
Let’s explore how AI/ML and automation improve data quality in healthcare.
1. Automating Data Capture
Manual data entry is prone to errors and inconsistencies. AI-powered tools automate data capture from multiple sources, such as EHRs and medical devices, reducing human input, minimizing mistakes, and enabling greater accuracy.
AI-driven data entry and ingestion improve data quality by extracting and processing both structured and unstructured data. Automated data capture ensures that all necessary fields are complete and accurate.
For example, Natural Language Processing (NLP) converts physician notes into structured data, preventing missing critical information. Optical Character Recognition (OCR) digitizes handwritten records and scanned documents, enhancing data completeness.
2. Detecting Data Errors
AI-powered systems enhance data quality by detecting errors and inconsistencies in large datasets. Even the slightest mistake can compromise data accuracy and usability.
Unlike manual monitoring, which relies on humans and is prone to errors, AI systems ensure that no mistakes slip through.
Many healthcare organizations now use machine learning models to analyze patterns, identify incorrect patient details, detect missing values, and flag coding errors that could impact clinical and operational decisions.
AI further strengthens this process by profiling data, recognizing anomalies, and addressing inconsistencies before they cause issues. By automating error detection, AI minimizes inaccuracies and ensures that healthcare data remains complete, reliable, and actionable.
3. Data Cleaning and Validation
AI-powered tools improve healthcare data quality by identifying and correcting duplicate, incomplete, or inaccurate patient records. This ensures data consistency across systems and prevents errors, that can lead to misdiagnoses and administrative delays.
ML algorithms analyze patterns in data, automatically flagging discrepancies before they cause issues. For example, AI-driven real-time error detection can reduce data inaccuracies by 60%, improving both clinical decision-making and operational efficiency.
By continuously learning from historical data, AI refines validation processes, enhances accuracy, and ensures healthcare providers have reliable, high-quality data for better patient outcomes.
4. Automation for Workflow Optimization
AI streamlines healthcare operations by automating repetitive administrative tasks, reducing staff workload, minimizing errors, and improving efficiency.
By now, we are aware that manual data entry is prone to errors and consumes valuable time. AI eliminates these issues by automating data capture, validation, and processing, ensuring accuracy and consistency.
AI automates billing, coding, and payment processing in revenue cycle management, reducing claim denials and accelerating reimbursements. Automated validation and compliance checks make claims processing seamless, reducing administrative bottlenecks.
Many hospitals have started using Robotic Process Automation (RPA) and have seen a significant drop in administrative burden.
AI also optimizes appointment scheduling, follow-ups, and inventory management, further boosting operational efficiency.
5. Predictive Analytics for Proactive Decision-Making
Predictive analytics, powered by AI and automation, can proactively address poor data quality in healthcare by identifying and correcting anomalies before they impact patient care.
By continuously analyzing data patterns, AI systems can detect inconsistencies or errors in real-time, allowing for immediate intervention and correction. This proactive approach not only enhances the accuracy of patient records but also supports informed decision-making, leading to improved clinical outcomes.
Implementing predictive analytics fosters a data-driven culture within healthcare organizations, ensuring that data quality issues are addressed promptly and do not compromise the integrity of healthcare operations.
Implementing AI & Automation in Healthcare: Where to Start?
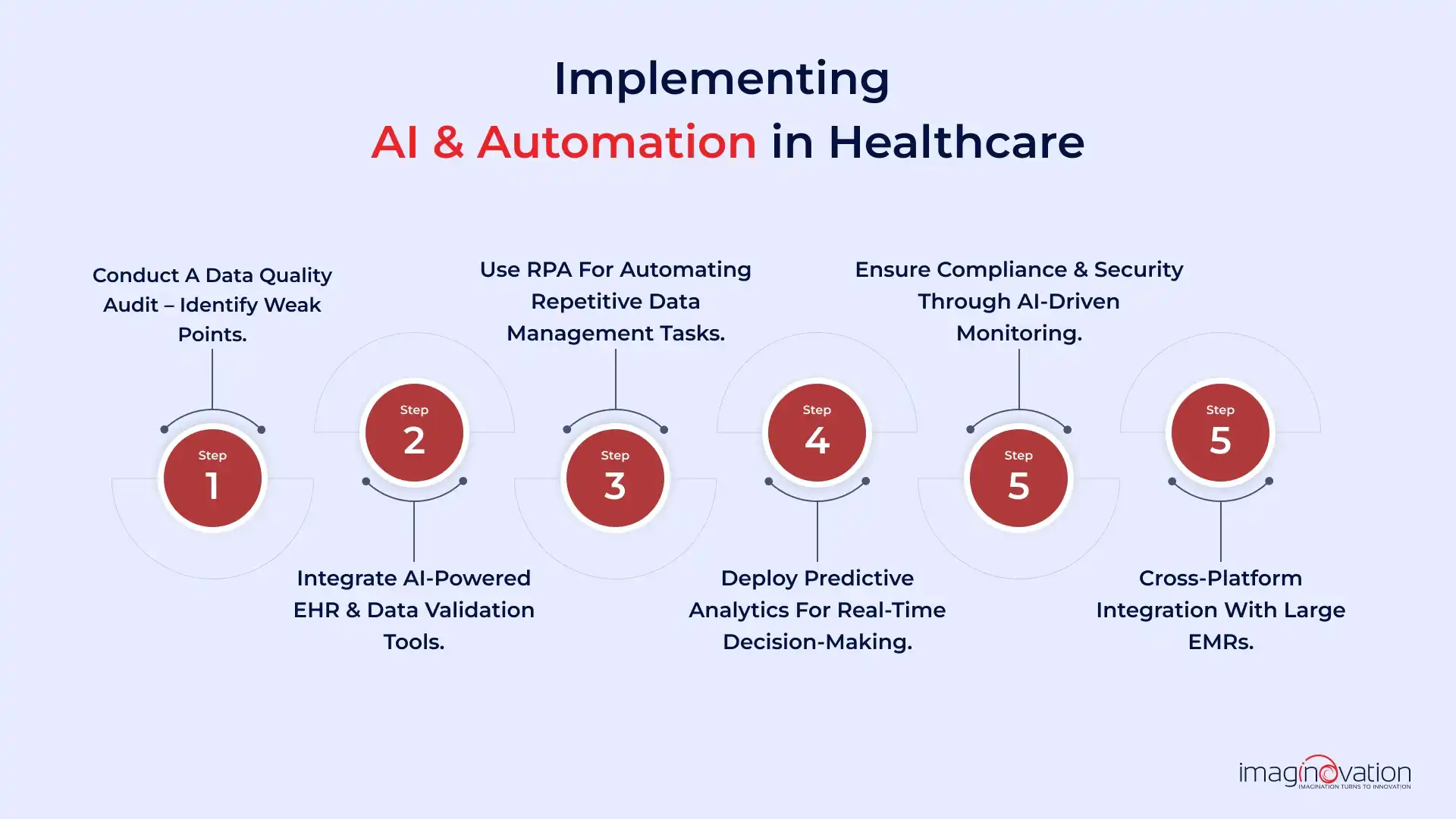
Adopting AI and automation in healthcare can revolutionize patient care and operational efficiency. Here’s a step-by-step guide to get started.
Step 1 - Conduct a Data Quality Audit – Identify Weak Points
The effectiveness of any AI system depends on the quality of the data it is trained on. AI models rely on accurate, relevant, consistent data to produce reliable results. Poor-quality data—whether inaccurate, incomplete, or irrelevant—leads to flawed decision-making and unreliable AI outputs.
Before building an AI model, you must assess the data quality and take steps to improve it. This includes data cleaning and preprocessing to remove errors, inconsistencies, and duplicate records. Additionally, data must accurately represent real-world scenarios.
For example, if your hospital is using AI to predict patient readmission rates, its dataset should include diverse patient demographics, medical histories, and treatment outcomes to ensure accurate forecasting. In cases of insufficient data, you may need to generate synthetic data to train the AI model effectively.
Step 2 - Integrate AI-powered EHR & Data Validation Tools
Once data quality is assured, the next step is integrating AI-powered Electronic Health Records (EHR) with advanced data validation tools. These integrations help maximize the accuracy and utility of healthcare data.
AI-powered EHR systems streamline data collection, integration, and validation, ensuring that information remains accurate, consistent, and reliable.
AI continuously monitors data for inconsistencies, helping you maintain high data integrity and improve patient outcomes.
Additionally, AI-driven validation tools ensure EHR data meets regulatory standards like HIPAA, reducing compliance risks and preventing data breaches. For example, predictive algorithms can analyze patient histories to forecast potential health risks, enabling proactive care.
Step 3 - Use RPA to Automate Repetitive Data Management Tasks
Robotic Process Automation (RPA) plays a crucial role in handling repetitive and time-consuming data management tasks in healthcare.
By automating routine processes like data entry, patient record updates, and claims processing, RPA reduces the burden on healthcare staff and minimizes human errors.
For example, instead of manually entering patient details across multiple systems, RPA bots can extract, validate, and update information in real time, ensuring consistency across databases. This automation saves time and improves data accuracy and compliance with healthcare regulations.
RPA enhances operational efficiency by automating billing, insurance verification, and appointment scheduling.
For instance, an RPA bot can automatically verify insurance details before a patient's visit, reducing delays. By leveraging RPA, healthcare organizations can streamline workflows, bring down administrative costs, and allow staff to focus on patient care.
Step 4 - Deploy Predictive Analytics for Real-time Decision-Making
Predictive analytics empowers healthcare providers to make proactive, data-driven decisions by analyzing real-time patterns and trends. By leveraging AI and machine learning, predictive models can assess patient data, identify potential health risks, and recommend timely interventions.
For example, hospitals can use predictive analytics to forecast patient admissions, helping them allocate resources efficiently and prevent overcrowding.
Similarly, AI-driven models can analyze a patient’s medical history to predict the likelihood of complications, allowing doctors to take preventive measures before issues escalate.
Beyond patient care, predictive analytics enhances operational efficiency by optimizing staffing schedules, managing inventory, and preventing equipment failures. F
Step 5 - Ensure Compliance & Security through AI-driven Monitoring
AI-driven monitoring helps healthcare organizations maintain compliance with regulations and protect sensitive patient data. With strict laws like HIPAA in the U.S. and GDPR in Europe, ensuring data security is critical to avoid legal penalties and maintain patient trust.
AI-powered systems can continuously monitor data access, detect anomalies, and flag potential security threats in real time.
For example, if an unauthorized user attempts to access patient records, AI can instantly trigger alerts and prevent breaches. These systems also help ensure that electronic health records (EHRs) adhere to regulatory standards by automatically validating data accuracy and completeness.
Step 6 - Cross-platform Integration with Large EMRs
For AI to deliver its full potential in healthcare, it must integrate seamlessly with large Electronic Medical Records (EMRs) and other digital health platforms.
Many healthcare providers use multiple systems to manage patient data, billing, and clinical workflows. Without proper integration, data silos can form, leading to data inconsistencies.
AI-powered integration tools enable smooth data exchange across different EMR platforms, ensuring that patient records remain consistent and up to date. For example, an AI-driven system can automatically sync lab results, prescriptions, and patient histories across hospitals, clinics, and pharmacies, reducing duplication and errors.
The ROI of AI-Powered Data Quality Improvement in Healthcare
Investing in better data quality leads to real financial and operational benefits for healthcare providers.
One of the primary benefits is faster claims approval and reimbursement processing. Automated systems capture, verify, and submit claims quickly, reducing errors and speeding up approvals, improving healthcare providers' cash flow. For example, an AI-powered claims system can flag missing patient details before submission, preventing costly resubmissions and delays.
AI also helps reduce operational costs. Healthcare facilities can save on staff salaries, training, and other administrative expenses by automating data entry, verification, and error correction. This ensures that resources are used more effectively.
Patient outcomes improve significantly with accurate data. AI systems continuously clean and update patient records, allowing doctors to make better-informed decisions. This leads to more effective treatments and quicker recoveries. For example, AI-powered alerts can notify doctors of potential drug interactions, preventing medical errors and ensuring patient safety.
With accurate data, doctors can make better decisions, leading to improved patient outcomes. AI-driven insights help predict risks, personalize treatments, and reduce unnecessary procedures. This leads to shorter hospital stays and better resource management.
Good data quality also ensures compliance with healthcare regulations. It reduces the risk of fines and legal issues caused by inaccurate or incomplete records. By preventing errors, healthcare organizations can avoid costly penalties and maintain patient trust. For example, AI systems can automatically audit patient records to ensure they meet HIPAA requirements, reducing the risk of compliance violations.
Conclusion
Poor data quality hinders healthcare by causing delays and limiting collaboration.
Imaginovation understands this and helps providers overcome these challenges with AI-driven automation, integrated analytics, and strong data governance.
Our solutions streamline workflows, enhance decision-making, and ensure accurate, reliable data for better patient care.
Partner with us to break down data silos, fix data quality issues, reduce costs, improve outcomes, and build a smarter, data-driven future.
Contact us today to get started.